Ayushman Bharat Digital Mission: A Reality Check
By Dr. Ritisha Nadia James
The ambitious ABDM has promising outcomes by creating a synchronized paperless system for capturing and storing healthcare data. However, some roadblocks need to be addressed urgently.
India delivers quality of care at par with North American and European counterparts and at one of the most affordable rates; however, the paper trail is endless. Modern countries are moving towards implementation of a common EHR that would be shared across different health exchange data, and India has finally hopped onto that bandwagon.
It is a known dilemma for doctors that previous notes from other healthcare professionals are often absent for a particular patient, thereby creating a disconnect in the patient’s medical history; which in turn leads to repeated tests and increase in out-of-pocket expenditure.
This concern has been recognized by the Ministry of Health, and in the National Health Policy of 2017, the framework for a digital health technology eco-system was proposed.
A pilot was done in six Union Territories (Andaman & Nicobar, Chandigarh, Dadra & Nagar Haveli and Daman & Diu, Ladakh, Lakshadweep and Puducherry), and on 27th September 2021, India launched the Ayushman Bharat Digital Mission (ABDM). NDHM was renamed to ABDM to ensure a commonality to the Ayushman Bharat Yojana scheme.
What does ABDM mean for the common man?
It is the digitization of health information, thereby creating a transparent and seamless system amongst different health entities. For this, firstly, a health account (Ayushman Bharat Health Account) is created for an individual, with a corresponding ABHA ID, which will also be linked to that person’s Aadhaar number. All healthcare entities (physicians, hospitals, etc.) are also required to register with ABDM. Once registered, individuals can then manage their health information via the ABHA app.
Unlike the field work done for the Aadhaar card, it is not compulsory for every Indian to create their ABHA account; inspite of the ABHA card being linked to Aadhaar number. One would think that this being part of the National Health Mission, it would be a mandatory exercise.
In order to ensure compliance from the healthcare entities, The National Health Authority (NHA) created the Digital Health Incentive Scheme (DHIS). As per the press release in December 2022, “Under the DHIS, the eligible health facilities and digital solutions companies shall be able to earn financial incentives of up to Rs. 4 crores based on the number of digital health records they create and link to ABHA.” This is over and above the approximate 1.4 billion rupees budget for NDHM.
As of date, there is no published record of the number of health entities currently with ABHM, but in July 2021, 23,300 hospitals were empaneled. In May 2022, a public dashboard was said to have been created to monitor the progress of hospitals being registered. However, this dashboard is currently not available for public viewing.
Under State regulations, Andhra Pradesh has claimed to be the first state to link over 1 Crore health records to ABHM, along with creation of 3.4 crore ABHA IDs. The A.P. government was able to achieve this feat with the help of Bengaluru-based healthcare consultancy firm, Medblocks; and along with the healthcare fieldworkers to get the personal details from the people.
While as a whole, it appears to be a fairly simple process of creating a health ID, and then uploading scanned copies of medical records onto the ABHA app, the ground reality of this process is fairly complex.
Dr. Sidharth Ramesh, Founder of Medblocks has shared some of the challenges encountered during the project. In the digital world, sharing of data is done through Fast Healthcare Interoperability Resources (FHIR), which is the standard for exchange healthcare information electronically; and is done with the help of API technology. An API is an Application Programming Interface, that sends signals between various programs in order to communicate, and thereby allowing the integration across different applications, programs, services or systems.
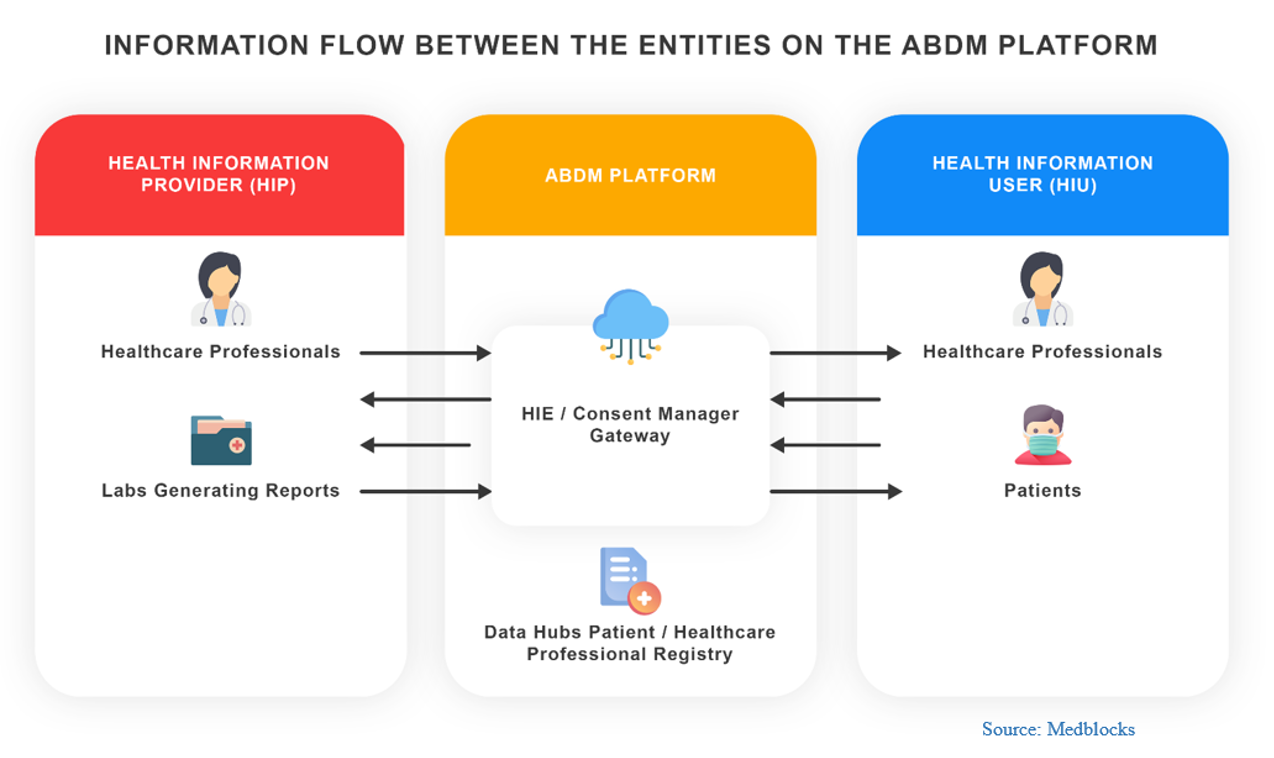
The ABDM architecture is built in the same way. Healthcare data can only be viewed if the owner of the data provides their consent.
In general, for an information exchange, there is one API through which there is a two-way flow. “However, in the ABDM eco-system, there are 5 different APIs required to transfer data to the ABHA platforms. Furthermore, they are asynchronous APIs which means that the data exchange may not be immediate; thereby, leading to a slow signal transmission.” Think of this as a highway with two-way traffic, but suddenly there are multiple detours in this highway to reach from destination A to destination B, thereby leading to delayed journey time. A single API is more efficient than having multiple. More is not always best!
“On top of that, Health Insurance APIs are different. The data exchange for Health Insurance companies comes separately under the ‘Insurance Exchange Protocols.”
The type of data shared is a ‘diagnostic summary’ that can be in any format. “User is able to use any code because there is no matching of content to the API. Since there is no data validation, this leads to data that is not meaningful. Security risk is also a concern.” What this means is that there are no set rules on how and in what manner the diagnostic information is to be shared. Random information can be shared, which may not be of any relevance to the patient diagnostic history.
The diagnostic summary is not the usual paper prescription that is given to patients. Data provided by healthcare entities would need to be converted into a digitized format which is using codes instead free text. The guidelines for this coding system are as per the Systematized Nomenclature of Medicine Clinical Terms (SNOMED CT) which is a system for classifying many types of medical data. It is the most widely recognised nomenclature in healthcare. It is different from ICD-10, which only includes classification of diseases, whereas SNOMED also covers procedures, symptoms, etc.
It is a known fact that most healthcare entities do not have a Medical Information Systems (MIS) in place, except for a handful tertiary care hospitals such as Apollo and Fortis. Most health insurance companies have been established after 2005, and they too, do not necessarily follow the SNOMED CT classification. For those who have absolutely no form of a MIS, it would be a mammoth task to convert the paper files, from inception, into the current coding practice as required by ABDM.
Dr. J.P. Pattanaik, a HL7 V2x and FHIR R4 certified consultant with Optum, believes that ABDM is a transformative initiative for India’s for digital health ecosystem. “However, while we have achieved significant success in storing operational data in digital format, capturing clinical information, and using terminology standards – we still have a long way to go. ABHA ID will do wonders only when we have enough clinical information at the source.”
“Government has proposed incentives for digital clinical information, but this may not be enough for addressing the challenges at the grassroots. Those who can’t afford to implement good Hospital Information Systems/Electronic Medical Records (EMR), should be assisted with clinician friendly minimum necessary opensource systems (OSS) for adapting and scaling this initiative. Thus, we still need to work on basic building blocks which will help in rapid adoption.” Not all physicians are tech savvy, and having to now convert age old paper prescriptions into data, would be another challenging task; hence we would need OSS, which have a simple user interface (UI) that physicians would understand, and support them on the EMR creation.
While we have analyzed the current technical issues with the implementation of ABDM, the bigger question to ask is – who is governing the entire process? Is there an authoritative body to ensure that the correct data is being uploaded in the correct format? Have the right security protocols been put in place? And how do you make sure that there is no identity theft or theft of data?
Having a digital healthcare ecosystem would definitely have a paradigm shift with a positive impact. With data at hand, reactive medicine can be converted to predictive medicine, giving way to an optimized delivery of care at affordable rates.